What Is Known About Pelvic Floor Dysfunction [PFD]?
Pelvic Floor Dysfunction results from compromised coordination of muscles supporting pelvic organs, leading to urinary, fecal, and sexual challenges. Causes include childbirth, aging, and trauma, with psychological factors often exacerbating symptoms.
Diagnosis entails medical history review, physical exams, and specialized tests like electromyography or urodynamic studies. Treatment focuses on addressing underlying causes and symptoms, typically involving pelvic floor physical therapy, medications, or surgery if necessary.
In women, symptoms may include urinary incontinence, pelvic organ prolapse, and sexual dysfunction, while men may experience urinary incontinence, erectile dysfunction, or pelvic pain.
Early detection and intervention are critical for improving quality of life. Healthcare providers, including urologists and pelvic floor therapists, collaborate to devise personalized treatment plans.
Raising awareness and fostering open discussions about pelvic floor health are vital to reduce stigma and enhance access to care.
By acknowledging the complexity of Pelvic Floor Dysfunction and advocating for comprehensive care approaches, healthcare professionals empower individuals to address their pelvic health concerns effectively.
Which Pelvic Floor Do You Have?
The pelvic floor comprises a network of muscles vital for providing support to various organs within the pelvic region. In individuals with uteruses, these muscles support the uterus, bladder, and colon, while in individuals with penises, they support the bladder and colon. The urethra, vagina, and anus serve as apertures within the pelvic floor.

Termed as pubococcygeus (PC) muscles, commonly referred to as pelvic floor muscles, these structures play a pivotal role in regulating urinary and fecal continence as well as contributing to certain aspects of sexual function.
Identifying Symptoms Associated with Pelvic Floor Dysfunction:
Symptoms indicative of Pelvic Floor Dysfunction encompass:
Difficulty urinating or defecating: Challenges in initiating or completing urination or bowel movements.
Sensation of incomplete bowel movements: Feeling as though bowel movements are not fully evacuated.
Urinary or fecal leakage: Involuntary discharge of urine or feces, leading to potential embarrassment or hygiene concerns.
Frequent urge to urinate: Persistent sensation of needing to void the bladder frequently.
Straining during urination or bowel movements: Effort required to initiate or complete the process of urination or defecation.
Intermittent urine flow: Starting and stopping of urine flow during urination.
Chronic constipation: Long-standing difficulty in passing stools, often accompanied by discomfort.
Altering positions to facilitate bowel movements: Needing to change positions to aid in the passage of stools.
Painful urination: Discomfort or pain experienced during the act of urination.
Unexplained lower back pain: Persistent or recurrent pain in the lower back region without a clear cause.
Genital, anal, or pelvic pain: Discomfort or pain localized in the genital area, anus, or lower abdomen/pelvic region, which lacks an obvious explanation.
Symptoms may differ between individuals with penises and those with vaginas. In women, Pelvic Floor Dysfunction can contribute to erectile dysfunction and may resemble prostatitis symptoms. This underscores the importance of precise clinical evaluation for accurate diagnosis and treatment.
Women experiencing Pelvic Floor Dysfunction may report dyspareunia or pain during sexual intercourse as a symptom.
Exploring the Etiology of Pelvic Floor Dysfunction:
Dysfunction of the pelvic floor may be inherited. Some people’s connective tissue and muscles are just weaker.
But other factors can also contribute to it, such as:
- a pelvic injury
- pelvic surgery
- Growing Older
- Being too heavy or fat
- Getting pregnant and giving birth
- Going to the restroom too frequently or exerting too much effort
Primary etiological factors contributing to Pelvic Floor Dysfunction in women include pregnancy, advancing age, and obesity. Even in cases of cesarean delivery, pregnancy alone can lead to alterations in the pelvic region due to physiological changes.
Moreover, individuals with neurological conditions such as Parkinson’s disease may encounter pelvic floor issues, as neurological impairments can disrupt the coordination of pelvic floor muscles governed by nerve control.
Diagnostic Approaches for Pelvic Floor Dysfunction:
You will be asked questions about your health by your doctor in order to identify Pelvic Floor Dysfunction . This will entail learning about your bowel habits, urinary tract infection history, and any other illnesses that may contribute to pelvic floor problems. If you’re a woman, your doctor might inquire about previous pregnancies and any pain you experience during intercourse.
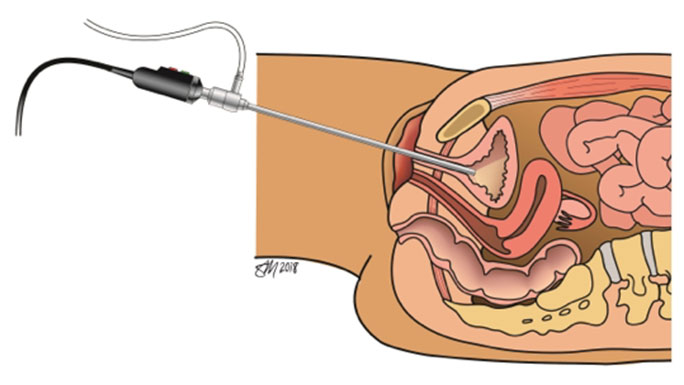
To check how your muscles are working, your doctor may use their fingers to complete an interior exam in addition to an outside inspection. To find out how well your pelvic floor muscles are functioning, there are further tests available.
Diagnostic procedures for Pelvic Floor Dysfunction may encompass the following:
Surface electromyography (EMG): Utilizing electrodes placed on the pelvic area surface to assess muscle function.
Anal manometry: Involves the insertion of a thin, flexible catheter with an uninflated balloon through the anus into the rectum to measure pressure movements during withdrawal.
Defecating proctogram: A radiographic examination involving the administration of a contrast enema to visualize muscle coordination and movement during defecation.
Uroflowmetry: A urodynamic test that measures the rate and volume of urine flow to evaluate bladder emptying efficiency during voiding episodes.
Treatment Strategies For Pelvic Floor Dysfunction:
The treatment approach for Pelvic Floor Dysfunction is individualized based on the severity of the condition and the specific symptoms experienced by the patient.
For individuals with overactive bladder, treatment options may include kegel exercises, topical estrogen cream, or prescription medications.

Kegel exercises entail the voluntary contraction and relaxation of pelvic floor muscles to enhance strength and control. A recommended regimen typically involves performing 10 to 20 repetitions, each lasting approximately five seconds, repeated three to four times daily. This regimen aims to strengthen the pubococcygeal muscles, thereby potentially alleviating symptoms associated with overactive bladder.
Fecal incontinence, a potential consequence of Pelvic Floor Dysfunction , arises when the musculature responsible for regulating bowel movements functions inadequately, resulting in involuntary leakage. Treatment strategies may encompass dietary modifications, pelvic floor exercises, or surgical interventions aimed at nerve stimulation within the pelvis or tightening the sphincter muscle.
Prolapse, a potential complication of PFD, manifests when the rectum or vagina descends from its normal position due to inadequate support from the pelvic floor musculature. While Kegel exercises may offer some benefit, surgical intervention stands as a primary treatment modality for prolapse.
General Medical Care. Treatments for PFD generally consist of:
Treatment modalities for PFD commonly involve:
- Pharmacotherapy: Utilization of muscle relaxants or other prescription medications to alleviate symptoms.
- Physical therapy: Implementation of tailored exercises and techniques to retrain and fortify pelvic floor musculature.
- Behavioral interventions: Incorporation of strategies to mitigate straining during voiding or defecation, often through cognitive and lifestyle adjustments.
- Lifestyle modifications: Adoption of practices such as yoga or hydrotherapy to promote relaxation and optimize pelvic floor muscle function.
Pelvic floor exercises, known as Kegel exercises, are beneficial for strengthening pelvic musculature irrespective of age or gender. They remain beneficial both pre- and post-pregnancy. Engaging in these exercises can also serve as a preventive measure against future PFD, particularly for individuals planning pregnancy or currently pregnant.
FQAs:
What treatment options are available for PFD?
Treatment may include pelvic floor muscle training (Kegel exercises), physical therapy, medication (such as muscle relaxants or topical estrogen), behavioral modifications, lifestyle changes (such as weight management), or surgical interventions depending on the severity and underlying cause of the disorder.
Can pelvic floor exercises prevent PFD?
Yes, performing pelvic floor exercises regularly, regardless of gender or age, can help strengthen the pelvic floor muscles and reduce the risk of developing PFD, especially for individuals planning pregnancy or currently pregnant.
Can PFD be cured?
While PFD may not always be completely cured, they can often be effectively managed with appropriate treatment and lifestyle modifications, leading to improved symptoms and quality of life. Early diagnosis and intervention are key to successful management.
When should I seek medical attention for pelvic floor symptoms?
Suppose you experience persistent or bothersome symptoms related to PFD such as urinary or fecal incontinence, pelvic pain, or pelvic organ prolapse. In that case, it is advisable to consult a healthcare professional for proper evaluation and management.
In conclusion:
“In conclusion, PFD presents challenges in pelvic muscle coordination, impacting urinary, bowel, and sexual functions. Diagnosis involves comprehensive evaluation by healthcare professionals, while treatments, including physical therapy, medications, and surgery, are tailored to individual needs for symptom management and improved quality of life.”


![What Is Known About Pelvic Floor Dysfunction [PFD]?](https://ayeshasaleemfemaleuro.com/wp-content/uploads/2024/02/pelvic-floor-disorder.jpg)