Cystocele (Fallen Bladder)
A cystocele happens when the tendons and muscles that hold up your bladder stretch or debilitate. You might see or feel tissue swell through your vaginal opening or experience issues peeing or embedding feminine items. Sex may likewise be agonizing. Treatment might incorporate fortifying your pelvic floor muscles or a medical procedure.
What is a cystocele?
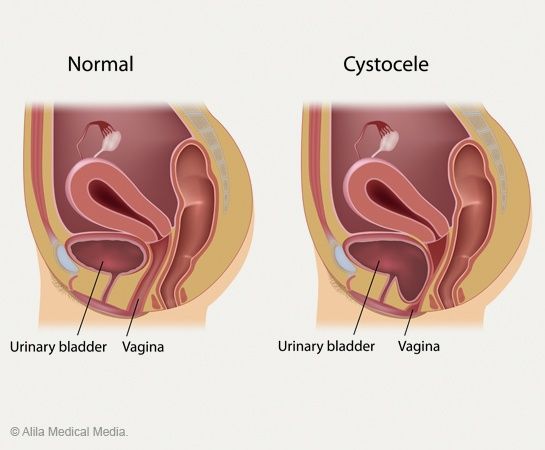
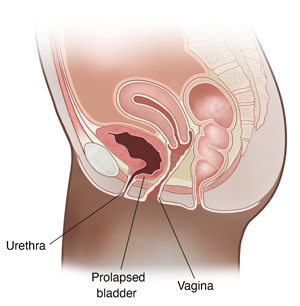
A Fallen Bladder, medically referred to as a cystourethrocele, is characterized by the weakening or stretching of the supportive ligaments and musculature surrounding the bladder and vaginal wall. This structural compromise results in the descent or sagging of the bladder into the vaginal cavity. Fallen Bladder is categorized as a form of pelvic organ prolapse, wherein the normal anatomical positioning of pelvic organs is disrupted due to compromised support structures.
Alternative designations for a Fallen Bladder (SIS-tuh-seel) encompass terms such as:
– Dropped bladder.
These descriptors are used interchangeably within medical discourse to denote the condition characterized by the descent or prolapse of the bladder into the vaginal cavity due to weakened supportive structures.
What are the types of cystoceles?
Fallen Bladder severity is typically categorized into three grades:
Grade 1 (mild): Characterized by a limited descent of the bladder into the vaginal canal.
Grade 2 (moderate): Involves a descent of the bladder to the vaginal opening or slightly protruding beyond it.
Grade 3 (severe): Manifests as a substantial protrusion of the bladder beyond the vaginal opening.
How serious is a cystocele?
The impact of a Fallen Bladder varies according to its severity. Patients may experience discomfort or urinary incontinence in cases of mild Fallen Bladder presentation. Conversely, severe Fallen Bladder can result in urinary retention, potentially leading to urinary tract infections or renal impairment. It is imperative to address Fallen Bladder severity promptly through medical assessment and appropriate management to mitigate associated risks and preserve urinary function and overall health.
How common is a cystocele?
Cystoceles are prevalent, with medical experts estimating that approximately 50% of females and individuals assigned female at birth (AFAB) experience some degree of Fallen Bladder
Symptoms and Causes:
What are the symptoms of a cystocele?

Symptoms associated with Fallen Bladder may comprise:
- Sensation or visualization of vaginal bulging.
- Perception of pelvic fullness, heaviness, or discomfort exacerbated by standing, lifting, coughing, or prolonged activity.
- Increased frequency of urination.
- Challenges in complete bladder emptying during urination.
- Recurrent urinary tract infections (UTIs).
- Difficulty with insertion of menstrual hygiene products, including tampons and menstrual cups.
What causes a cystocele?
Fallen Bladder typically result from the stretching or weakening of pelvic ligaments, which can be attributed to various factors, including:
- Vaginal childbirth potentially exerts strain on pelvic floor muscles.
- Familial predisposition t Fallen Bladder
- Obesity is characterized by a body mass index (BMI) exceeding 30.
- Undergoing hysterectomy.
- Decline in estrogen levels, commonly associated with aging and menopause. Estrogen plays a crucial role in maintaining the strength of muscles surrounding the vaginal area. With advancing age and the onset of menopause, estrogen production decreases, potentially contributing to pelvic floor weakening.
Who do cystoceles affect?
Fallen Bladder can affect individuals with a vagina across all age groups. However, the likelihood of developing a Fallen Bladder increases with age due to the progressive weakening of pelvic floor muscles. Additionally, the following factors can heighten the risk of Fallen Bladder development:
- Vaginal childbirth.
- Undergoing pelvic floor muscle or uterine surgeries, including hysterectomy.
- Obesity.
- Familial predisposition to Fallen Bladder.
What are the complications of a cystocele?
A cystocele has the potential to exert pressure on the urethra, leading to urinary retention, wherein the bladder is unable to fully empty during urination. Furthermore, a Fallen Bladder may cause torsion or twisting of the ureters, the conduits responsible for transporting urine from the kidneys to the bladder. Accumulation of urine in the kidneys due to obstruction or impairment in urine flow can result in renal damage.
Diagnosis and Tests:
How are cystoceles diagnosed?
A healthcare professional specializing in the female reproductive and urinary systems, such as a urologist or gynecologist, is equipped to diagnose a Fallen Bladder. The diagnostic process typically involves thoroughly reviewing the patient’s medical history, a comprehensive symptom assessment, and a physical examination.
In addition to these steps, the healthcare provider may recommend the following diagnostic tests:
- Urodynamic testing: This assessment evaluates the bladder’s functionality, assessing its capacity to retain and expel urine effectively.
- Cystoscopy: During this procedure, a healthcare provider inserts a slender, illuminated tube with a camera at its tip (cystoscope) through the urethra into the bladder. This allows for direct visualization of the urinary tract to identify abnormalities such as malformations, obstructions, tumors, or stones.
How do I check myself for a cystocele?
Diagnosis of a Fallen Bladder requires assessment by a healthcare professional. However, individuals may experience a protrusion from the vaginal opening and may be able to manually reduce it. Prompt medical evaluation is crucial upon experiencing symptoms suggestive of a Fallen Bladder.
Management and Treatment:
How do you get rid of a cystocele?
The severity of your cystocele will determine this.
The only treatment you might need if you have a moderate Fallen Bladder that doesn’t affect you is to avoid hard lifting or straining, as these activities can exacerbate the Fallen Bladder.
Additional approaches for treating mild Fallen Bladder include:
Keeping yourself at a healthy weight.
Treatment with estrogen replacement.
To strengthen your urethra, vagina, and rectum, perform Kegel exercises.
A pessary gadget to assist with bladder retention.
If the preceding methods are ineffective for treating a moderate or severe Fallen Bladder , surgery may be necessary.
What happens during and after surgery for a cystocele?
For individuals with moderate to severe Fallen Bladder, anterior colporrhaphy may be recommended as a reconstructive surgical intervention. During this procedure, the surgeon repositions the bladder to its normal anatomical location and tightens the anterior vaginal wall muscles to provide support.
Typically performed as an outpatient procedure, Fallen Bladder surgery allows patients to return home on the same day of the operation. Most individuals experience a complete recovery within a few months post-surgery.
In cases where sexual intercourse is not anticipated in the future, surgical options exist to close and shorten the vaginal canal, eliminating bulges.
If the pelvic organ prolapse extends beyond the bladder, involving structures such as the uterus, vaginal apex (post-hysterectomy), or rectum, alternative surgical approaches may be discussed by the healthcare provider.
How soon after treatment will I feel better?
If surgery is necessary for a serious Fallen Bladder, you should recover quickly. However, it can take a few weeks to fully recover.
Prevention:
Can a cystocele be prevented?
Several Fallen Bladder risk factors are modifiable through proactive lifestyle choices and behavior modifications, including:
- Maintaining an optimal body weight: Consultation with a healthcare provider regarding personalized weight management strategies is advisable to promote overall health and reduce Fallen Bladder risk.
- Preventing constipation: Adopting a high-fiber diet, adequate hydration, and regular physical activity can help mitigate constipation risk factors.
- Safeguarding pelvic floor muscles during strenuous physical exertion: Practice lifting techniques, such as squatting with hip and knee flexion while keeping the back straight, to minimize strain on pelvic floor muscles.
However, certain risk factors, such as family history and advancing age, are non-modifiable. Despite lifestyle modifications, it’s important to acknowledge that these factors may contribute to Fallen Bladder development. Regular consultation with a healthcare provider is essential for comprehensive risk assessment and appropriate preventive measures.
Outlook / Prognosis:
What is the outlook if I have a cystocele?
Cystoceles are not considered life-threatening; however, they can significantly impact one’s quality of life. Without proper treatment, Fallen Bladder have the potential to exacerbate, leading to urinary retention, a condition where individuals may experience difficulty urinating. In severe cases, urinary retention can predispose individuals to urinary tract infections and renal damage. It is imperative to address Fallen Bladder promptly to prevent potential complications and preserve urinary function and renal health. Regular consultation with a healthcare professional is essential for timely diagnosis and appropriate management of Fallen Bladder
Living With
What should I avoid if I have a cystocele?
Individuals diagnosed with a Fallen Bladder are advised to refrain from engaging in activities that impose excessive strain on the pelvic floor muscles, particularly heavy lifting or activities that increase intra-abdominal pressure.
Furthermore, it is recommended to address and manage conditions contributing to chronic coughing, such as bronchitis, as prolonged coughing can exert significant pressure on the chest and abdomen, resulting in strain on the pelvic floor muscles. Smoking cessation and seeking appropriate treatment for underlying respiratory conditions are integral components of Fallen Bladder management to mitigate the risk of exacerbating pelvic floor dysfunction.
When should I see a healthcare provider?
Consult a medical professional if you experience Fallen Bladder symptoms, particularly if they negatively impact your quality of life.
When should I go to the ER?
If you can’t urinate and have symptoms of a Fallen Bladder visit the emergency hospital.
What questions should I ask a healthcare provider?
How would you realize I have a Fallen Bladder?
What other condition do I have if I don’t have a Fallen Bladder?
What treatment do you suggest?
Could I, at any point, deal with a Fallen Bladder without a medical procedure?
Could I, at any point, seek a Fallen Bladder once more after treatment?
What exercises or developments are a good idea for me to avoid?
Could I, at any point, actually engage in sexual relations on the off chance that I have a cystocele?
Would it be a good idea for me to see a gynecologist or urologist?
Additional Common Questions:
What is the difference between a prolapsed bladder and a cystocele?
Fallen Bladder and prolapsed bladder are the same condition. Cystocele is also known as a prolapsed bladder.
A note from “THE KIDNEY CENTER”
While Fallen Bladder typically pose no immediate danger to one’s health, they can significantly impact an individual’s emotional well-being, leading to feelings of embarrassment or self-consciousness. It is important not to delay seeking medical attention if Fallen Bladder symptoms adversely affect your quality of life. A healthcare provider will thoroughly review your medical history and symptoms to formulate the most suitable treatment approach tailored to repair the Fallen Bladder and enhance overall well-being. Prompt consultation with a healthcare professional is essential to address Fallen Bladder-related concerns and ensure optimal management of symptoms.