What Is Kidney Cancer?
Kidney cancer, medically termed renal cancer or renal cell carcinoma (RCC), is characterized by the malignant proliferation of kidney cells, leading to the formation of tumors. Typically originating in the tubules of the kidney’s lining, renal cancer primarily manifests as renal cell carcinoma.
Renal cell carcinoma accounts for the majority of kidney cancer cases and is frequently diagnosed before metastasis to distant organs occurs. Early detection facilitates more successful treatment outcomes, although kidney tumors may attain considerable size before diagnosis.
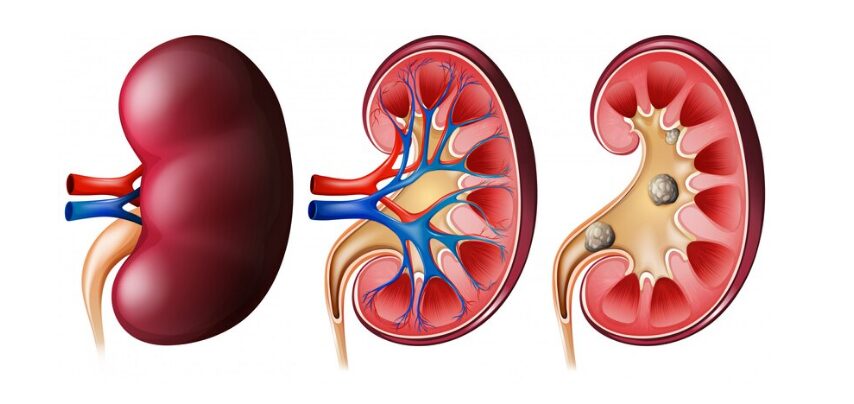
The kidneys, two organically shaped structures resembling beans and located bilaterally in the abdominal cavity alongside the spine, fulfill crucial functions in blood filtration and urine production.
Although the precise etiology of renal cancer remains elusive, several risk factors have been identified. Notably, renal cancer incidence is higher among individuals aged 40 and older. Other recognized risk factors include:
- Smoking: Individuals who smoke cigarettes or cigars are at a significantly higher risk of renal cancer compared to nonsmokers.
- Gender: Men have a higher susceptibility to renal cancer, with approximately double the risk compared to women.
- Obesity: Excess weight can lead to hormonal changes that elevate the risk of developing renal cancer
- Prolonged Use of Certain Pain Medications: Extended usage of specific pain medications, both over-the-counter and prescription drugs, may increase the likelihood of renal cancer
- Advanced Kidney Disease or Long-term Dialysis: Individuals with advanced kidney disease or undergoing prolonged dialysis treatment are at an increased risk of renal cancer
- Genetic Conditions: Conditions such as von Hippel-Lindau (VHL) disease or inherited papillary renal cell carcinoma can predispose individuals to renal cancer
- Family History: Having a family history of renal cancer, particularly among siblings, significantly elevates the risk of developing the disease.
- Exposure to Certain Chemicals: Occupational or environmental exposure to substances such as asbestos, cadmium, benzene, organic solvents, and specific herbicides can contribute to an increased risk of renal cancer.
- High Blood Pressure: While the relationship between high blood pressure and renal cancer risk is not fully understood, individuals with hypertension may have an elevated risk.
- Race: Black individuals have a slightly higher risk of renal cancer compared to white individuals, although the reasons for this disparity are not well-established.
- Lymphoma: Patients with lymphoma may have an increased risk of renal cancer although the underlying cause of this association is currently unknown.
Renal cancer is not guaranteed to occur in those who have these risk factors. Not having any of them does not prevent you from contracting the illness, either.
What Are the Symptoms of Kidney Cancer?
In numerous instances, individuals may not exhibit early symptoms of kidney cancer. As the tumor progresses in size, symptoms may gradually manifest. Individuals experiencing renal cancerr may present with one or more of the following symptoms:
- Hematuria (blood in the urine)
- Abdominal or flank mass
- Anorexia (loss of appetite)
- Persistent flank pain
- Unexplained weight loss
- Prolonged fever unrelated to infections
- Severe fatigue
- Anemia
- Peripheral edema (swelling in the ankles or legs)
Other symptoms that renal cancer may produce if it spreads to other places in your body include:
- Dyspnea (shortness of breath)
- Hemoptysis (coughing up blood)
- Skeletal pain (bone pain)
How Do I Know If I Have Kidney Cancer?
Perhaps you have experienced side discomfort, loss of weight, or excessive weariness as indications of renal cancer. Alternatively, it could be that during a normal examination, your doctor discovered a lump on your side or that a test for another illness revealed renal cancer. Nevertheless, a complete physical examination, a complete medical history, and diagnostic testing are required to confirm a renal cancerr diagnosis.
Your doctor will check for fever and high blood pressure and feel your side and belly for lumps. In addition, you will be asked about your medical history, current medical conditions, and previous treatments. Your doctor may additionally prescribe one or more of the following tests to diagnose renal cancer:
Urine Tests: Urinalysis is conducted to detect the presence of blood or other abnormalities in the urine, which may indicate kidney dysfunction or the presence of tumors.
Blood Tests: Blood chemistry tests assess kidney function and detect abnormalities in kidney function markers.
Intravenous Pyelogram (IVP): This imaging procedure involves the intravenous administration of a contrast dye followed by X-ray imaging to visualize the urinary tract and identify any abnormalities or tumors.
Ultrasound (Renal Ultrasonography): Ultrasonography utilizes sound waves to generate images of the kidneys, aiding in assessing kidney structure and detecting any solid or fluid-filled masses indicative of tumors.
Computed Tomography (CT) Scan: CT scanning employs X-rays and computer technology to produce detailed cross-sectional images of the kidneys, providing precise visualization of any tumors or abnormalities. Contrast dye may be administered intravenously to enhance image quality.
Magnetic Resonance Imaging (MRI): MRI utilizes powerful magnets and radio waves to create detailed images of kidney tissues, facilitating the detection and characterization of tumors. Contrast agents may be injected to enhance image contrast and clarity.
Renal Arteriogram: This specialized imaging test evaluates the blood supply to kidney tumors by visualizing the renal arteries. While not commonly performed, it may be utilized to diagnose small tumors or assess vascular involvement.
In many cases, a definitive diagnosis of renal cancer can be established based on clinical evaluation and imaging studies, obviating the need for a biopsy. However, in certain instances, a biopsy may be performed to confirm the diagnosis and assess the aggressiveness of the cancer.
A needle biopsy procedure may be employed to extract a tissue sample from the suspected tumor site, which is subsequently examined microscopically for the presence of cancer cells. Additionally, the biopsy results may provide insight into the grade of the cancer, indicating its aggressiveness and potential for metastasis.
Alternatively, surgical resection of the entire tumor may be undertaken, followed by histopathological examination of the excised tissue to confirm the diagnosis.
Following the confirmation of renal cancer, further diagnostic tests may be necessary to evaluate the extent of disease spread, a process known as staging. Imaging studies such as CT scans and MRI scans may be utilized to assess intrarenal involvement, contralateral kidney status, and potential metastasis to distant organs or tissues. A chest X-ray may also be performed to evaluate lung involvement, while a bone scan can detect bone metastases.
These diagnostic assessments are integral in determining the stage of renal cancer facilitating treatment planning, and guiding prognostic predictions.
What Are the Stages of Kidney Cancer?
The stages of renal cancer are categorized based on the extent of tumor growth and spread. The primary staging system used for renal cancer is the TNM system, which evaluates the size of the tumor (T), the involvement of nearby lymph nodes (N), and the presence of distant metastasis (M). The stages of renal cancer include:
Stage I:
The tumor is confined to the kidney and is ≤7 centimeters in size (T1), and has not spread to nearby lymph nodes (N0) or distant sites (M0).
Stage II:
The tumor is larger than 7 centimeters but remains confined to the kidney (T2), with no lymph node involvement (N0) or distant metastasis (M0).
Stage III:
The tumor has spread beyond the kidney to nearby tissues or lymph nodes but has not yet metastasized to distant sites. This stage is further subdivided into:
The tumor has invaded nearby tissues or spread to nearby lymph nodes but not beyond the Gerota’s fascia (T3a, N0, M0).
The tumor has extended beyond the kidney and Gerota’s fascia and may involve nearby lymph nodes (T3b/c, N0/N1, M0).
Stage IV:
The tumor has metastasized to distant organs or tissues, such as the lungs, bones, or brain, regardless of the size of the primary tumor or lymph node involvement (T any, N any, M1).
Understanding the stage of kidney cancer is critical for treatment planning and prognosis assessment. Treatment strategies vary depending on the stage of the disease, with early-stage tumors typically treated with surgery and localized therapies, while advanced-stage tumors may require systemic treatments such as targeted therapy, immunotherapy, or chemotherapy.
What Are the Treatments for Kidney Cancer?
Upon receiving a diagnosis and determining the stage of renal cancer, collaborative planning of treatment between the patient and their healthcare provider becomes paramount. Patients may gather additional information to facilitate an informed decision-making process. Referral to a specialist, such as a urologist, medical or radiation oncologist, or surgeon, for tailored treatment approaches, is common practice.

Before initiating treatment, seeking a second opinion regarding both the diagnosis of renal cancer and the proposed treatment regimen is often beneficial.
Renal cancer occasionally exhibits spontaneous regression, resulting in a return to an earlier stage; however, this phenomenon is infrequent, with an approximate incidence of 0.5%.
Various standard treatment modalities exist for renal cancer, with surgery typically serving as the primary intervention. Even in cases where surgical excision removes the entire tumor, adjunctive therapies may be recommended to eradicate any residual cancerous cells that evade detection.
Surgery for kidney cancer:
The primary surgical interventions for renal cancer encompass radical nephrectomy, simple nephrectomy, and partial nephrectomy, each tailored to the specific stage and characteristics of the disease.
Radical nephrectomy involves the excision of the affected kidney, adrenal gland, and adjacent tissue, often including nearby lymph nodes. It stands as the predominant surgical approach for renal cancer and has evolved to incorporate minimally invasive techniques, such as laparoscopy, enabling smaller incisions for enhanced patient recovery.
Simple nephrectomy entails the removal of solely the affected kidney, sparing adjacent structures.
Partial nephrectomy involves the surgical resection of the cancerous lesion within the kidney along with a margin of surrounding tissue. This approach is typically reserved for patients with smaller tumors (typically less than 4 cm) or in instances where a radical nephrectomy might jeopardize the function of the contralateral kidney.
If surgical resection is not feasible for renal cell carcinoma, alternative therapeutic modalities may be considered to achieve tumor destruction or control.
These may include nephron-sparing approaches such as partial nephrectomy, ablative techniques like radiofrequency or cryoablation, or systemic therapies such as targeted molecular agents or immunotherapy, depending on the patient’s clinical presentation and tumor characteristics.
Additionally, in cases where renal function is compromised due to bilateral kidney involvement or surgical intervention, renal replacement therapies such as dialysis or kidney transplantation may be necessary to maintain adequate renal function and overall patient health.
Cryotherapy employs cryogenic temperatures to induce tumor necrosis.
Radiofrequency ablation utilizes high-frequency radio waves to thermally ablate the tumor.
Arterial embolization entails the transcatheter insertion of embolic agents into the renal artery to induce tumor devascularization, often employed as a neoadjuvant intervention to reduce tumor size preoperatively.
Biologic therapy for Renal cancer:
Immunotherapy leverages the body’s immune system to combat cancer by enhancing, directing, or restoring its inherent defense mechanisms.
Biologic agents utilized in this therapeutic approach are naturally produced within the body or manufactured in laboratories.
Examples of biological therapies employed in treating metastatic renal cancer include interferon alpha and interleukin-2. Ongoing research efforts actively explore numerous novel immunotherapeutic strategies tailored specifically for managing renal cancer.
Targeted therapy for kidney cancer
Targeted therapy involves administering drugs or other substances designed to specifically identify and attack cancer cells while minimizing harm to normal cells. One category of targeted therapy is anti-angiogenic agents, which impede the formation of blood vessels that supply nutrients to tumors, resulting in tumor regression or halted growth.
Another category includes multikinase or tyrosine kinase inhibitors, orally administered drugs that inhibit enzymes critical for cancer cell proliferation.
Additionally, mTOR inhibitors, available in oral and intravenous forms, obstruct pathways essential for facilitating tumor cell growth by impeding blood vessel support. Each of these targeted therapies plays a distinct role in managing advanced renal cancer, offering diverse mechanisms of action and therapeutic benefits.
Radiation therapy for kidney cancer:
Radiation therapy is frequently employed to alleviate symptoms associated with renal cancer or in patients for whom surgical intervention is not feasible.
This treatment modality involves using high-energy X-rays or other forms of radiation to eradicate cancer cells or impede their proliferation. External radiation therapy directs radiation beams at the cancerous tissue from a machine positioned outside the body, facilitating precise targeting of the affected area while minimizing exposure to surrounding healthy tissue.
Chemotherapy for kidney cancer:
Chemotherapy involves the administration of drugs aimed at either destroying cancer cells or inhibiting their ability to multiply.
While chemotherapy is generally less effective for renal cancer compared to other cancer types, it may be utilized primarily for a specific subtype of renal cancer characterized by the presence of spindle cells, known as the sarcomatoid variant. In these cases, chemotherapy may be a comprehensive treatment approach to manage the disease.
How Can I Prevent Kidney Cancer?
While the precise causes of renal cancer remain unidentified, there are certain risk factors associated with the disease. Although prevention strategies are not yet well-defined, individuals can proactively mitigate risk. These steps include smoking cessation, maintaining a healthy body weight, effectively managing blood pressure, and minimizing exposure to potentially harmful chemicals. By adopting these lifestyle modifications, individuals may reduce their likelihood of developing renal cancer
FAQs:
What are the risk factors for kidney cancer?
The risk factors for renal cancer include smoking, obesity, high blood pressure, certain inherited conditions (such as Von Hippel-Lindau syndrome), and exposure to certain chemicals (such as cadmium or asbestos).
What are the symptoms of kidney cancer?
Symptoms of renal cancer may include blood in the urine, side or back pain, abdominal lumps, fatigue, weight loss, and loss of appetite.
How is kidney cancer diagnosed?
Renal cancer is typically diagnosed through a combination of medical history review, physical examination, imaging tests (such as ultrasound, CT scan, or MRI), and biopsy. If renal cancerr is suspected based on symptoms or imaging findings, a biopsy may be performed to confirm the diagnosis by examining a tissue sample from the kidney under a microscope.
Additionally, blood and urine tests may be conducted to assess kidney function and detect any abnormalities that could indicate the presence of cancer.
IN SUMMARY:
Diagnosing renal cancer typically involves several steps. It starts with a review of the patient’s medical history and a physical examination to look for signs and symptoms.
Imaging tests such as ultrasound, CT scans, or MRIs are commonly used to visualize the kidneys and identify abnormalities. If a suspicious mass is found, a biopsy may be performed, where a small sample of tissue is taken from the kidney and examined under a microscope to confirm the presence of cancerous cells.
Blood and urine tests may also be conducted to assess kidney function and identify any markers that could suggest the presence of cancer. This comprehensive approach helps healthcare providers diagnose renal cancer accurately and develop an appropriate treatment plan tailored to the patient’s needs.